A Denial Prevention Plan: Get What You Totally Deserve – Zee Medical Billing
Don’t Miss Out on What’s Yours – Let Us Ensure You Get Every Penny You Deserve. Trust Zee Medical Billing for Comprehensive Denial Prevention and Claim Success.
In medical billing, the most frequent challenge that each organization faces is claim denials. Denials in medical billing occur when claims are rejected by insurance companies for various reasons. A study indicates that around 30% of healthcare leaders say that claims denials are rising at a pace of 10% to 15% every day. But have you thought about why these denials are increasing? What are the causes behind their occurrence?
These causes can involve anything from straightforward coding or billing mistakes to more complicated problems like missing pre-authorization or insufficient patient data. No matter what the reason, rejections can lead to lower cash flow for healthcare providers, longer payment delays, and more administrative expenses.
But a good thing here is that about 63% of denials can be recovered but can be reworked rarely. Proper denial management is important to stop these increasing crises.
Why is it important to manage the denials?
Whenever one claim is denied it does not mean you just denied a claim it shows that you lost an opportunity which ultimately results in a loss of revenue. Healthcare providers must have a rejection prevention plan in place to reduce the negative effects of denials on their revenue cycle. Providers can dramatically lower the amount of denied claims and strengthen their financial position by recognizing frequent denial causes and taking proactive steps to fix them.
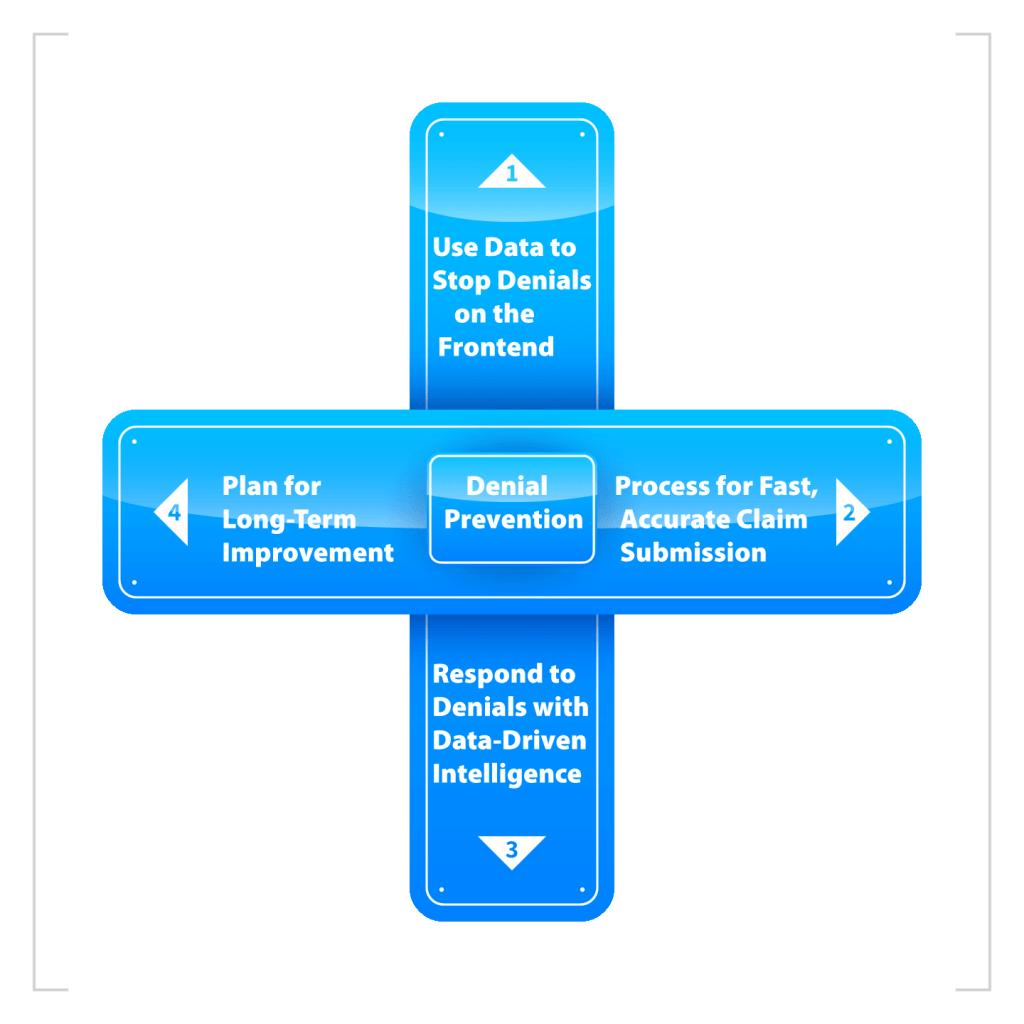
A strong denial reduction strategy can improve accuracy, streamline the billing process, and ultimately raise patient satisfaction. That’s why as an experienced company in the field of medical billing Zee Medical Billing has created a comprehensive 4-step denial prevention method in order to effectively deal with these denials challenges.
Steps to Manage Denials
- Step 1
- Step 2
- Step 3
- Step 4
Use Data to Stop Denials on the Frontend
At Zee Medical Billing, we understand that taking proactive front-end steps is the first step toward reducing denials. Effective data use is our first line of defense against denial issues as we recognize how critical it is to fix them.
Finding the Main Reasons for Denials
According to research the nearly 40% of denials are exclusively due to authorization problems, with 60% of denials resulting from problems at the beginning of the billing process. This emphasizes how crucial it is to address these problems early on in order to reduce rejections and increase income.
Activating Real-Time Eligibility Checks
A crucial aspect of preventing denials is ensuring that patients have eligibility for the services they receive. Real-time eligibility checks enable healthcare providers to verify a patient’s insurance coverage instantly, minimizing the risk of denials due to coverage issues. According to CAQH, the manual coordination of benefits costs the industry over $800 million annually, exacerbating the problem.
Solution
To effectively address this challenge, it’s essential to implement a solution that automates eligibility checks and provides staff with access to accurate, real-time eligibility information at the point of service. By leveraging technology, healthcare organizations can streamline the verification process and reduce the likelihood of denials stemming from eligibility issues.
Leverage Enriched Payer Responses
Inconsistencies or errors in payer responses are another frequent reason for rejections. Without proper data normalization and analysis, healthcare providers can find it difficult to identify and resolve these problems effectively.
Solution
To overcome this challenge, healthcare organizations should seek a solution that offers response and data normalization, allowing for the seamless integration and interpretation of payer responses. Comprehensive eligibility information that integrates data from payer websites and Electronic Data Interchange (EDI) transactions is essential for effectively fighting frontend denials.
Uncover Hidden Coverage
To address this challenge, healthcare organizations should adopt a solution that leverages payer connections and past claim data to quickly and accurately detect additional coverage. By automating the detection process, and addressing inaccuracies, organizations can identify unknown coverage promptly and prevent denials resulting from overlooked insurance benefits.
Solution
To overcome this challenge, healthcare organizations should seek a solution that offers response and data normalization, allowing for the seamless integration and interpretation of payer responses. Comprehensive eligibility information that integrates data from payer websites and Electronic Data Interchange (EDI) transactions is essential for effectively fighting frontend denials.
Automate Authorizations
Obtaining prior authorizations for medical services is a time-consuming process that can lead to delays and denials if not managed efficiently. Automating the authorization process can streamline operations, reduce inefficiencies, and reduce the risk of denials due to authorization-related issues.
Solution
To automate authorizations effectively, healthcare organizations should implement a solution that verifies, initiates, statuses and retrieves comprehensive authorization details automatically. By automating these processes, organizations can save time on manual tasks and ensure that all necessary authorizations are obtained promptly, minimizing the risk of denials.
Create a Process for Fast, Accurate Claim Submission
At Zee Medical Billing, we understand that the window between a patient visit and claim submission is critical in preventing denials. A very crucial stage that is often disregarded is the implementation of effective processes to guarantee a seamless transition and maximize the possibility of a clean claim submission. Let’s see this in detail:
Enhance Yield with Flexible Claim Edits
Correct claim edits are essential for ensuring the accuracy of claims submitted. However, the dynamic nature of payer guidelines, coupled with evolving rules and regulations, can pose challenges to maintaining effective claim edit processes. Zee Medical Billing emphasizes the importance of a robust claim edit library, complemented by the flexibility to create and manage custom edits tailored to the organization’s specific needs and to get the results in the form of:
- Increased percentage of first-pass clean claims
- Total number of clean claims
- Time saved researching payer guidelines and creating edit rules
- significant decrease in denials
By staying abreast of changing payer rules and guidelines, both internally and through collaboration with clearinghouse partners, healthcare providers can optimize claim submission processes and minimize denials.
Activate Automated, Paperless Enrollment
Traditionally, enrollment procedures have been seen to be cumbersome and time-consuming, especially when switching suppliers or adding new payers. However, Zee Medical Billing believes that with the right strategies in place, enrollment can be streamlined to minimize cash flow interruptions and resource strain. By embracing automated, paperless enrollment methods, healthcare organizations can simplify the transition process for all stakeholders involved.
Leverage Electronic Claim Attachments
Missing medical documentation is a common cause of denials, yet it is entirely avoidable with the right safeguards in place. Zee Medical Billing recommends leveraging electronic claim attachments to identify and address claims requiring additional documentation before submission. By automating what was once a manual, paper-based process, electronic claim attachments not only enhance efficiency by saving staff time but also facilitate quicker reimbursement and reduce denials associated with missing documentation.
Automate Coverage Verification
Even with accurate processes in place, the risk of submitting a claim with inactive or inaccurate coverage remains. To mitigate this risk, Zee Medical Billing advocates for the implementation of automated coverage verification solutions. By automatically identifying and updating coverage details prior to claim submission, healthcare organizations can significantly reduce eligibility-related denials and improve overall claims accuracy.
Respond to Denials with Data-Driven Intelligence
At Zee Medical Billing, we believe that the best way to handle rejections and improve revenue cycle management is to use data-driven insight. By leveraging data analytics and automation, healthcare organizations can proactively address denials, prioritize workflows, and improve overall financial performance.
Customize Your Status-Check Schedule
Traditionally, organizations base their decision to status a claim on either the number of days at the payer or the average remit date. While both approaches have merit, they can be limiting. Zee Medical Billing supports a status check methodology that is more adaptable and data-driven. By customizing the status-check schedule based on a comprehensive analysis of various data points, healthcare providers can avoid status checks that are either too early or too late, thereby increasing the likelihood of timely reimbursement.
Use Predictive Analytics to Prioritize Workflows
The wealth of data available to healthcare organizations presents an opportunity to prioritize workflows more effectively. By leveraging predictive analytics tools, providers can identify patterns and trends in denial data to prioritize their efforts on high-value items most likely to result in payment. Automation plays a crucial role in this process, streamlining workflows, reducing write-offs, improving visibility, and ultimately increasing appeal-conversion rates.
Automate Appeals and Go Paperless
Responding promptly to denials is essential in mitigating their negative impact on revenue. Zee Medical Billing recommends utilizing intelligent automation and advanced workflows to expedite the appeals process. By reviewing all denials within 72 hours and taking action within 7 days, healthcare organizations can foster a culture of efficiency and accuracy in denial management. Embracing paperless solutions further enhances workflow efficiency and reduces manual errors.
Install a Coverage-Detection Safety Net
In an ideal scenario, every claim submitted would be clean, and payers would process them promptly. But until that happens, it’s critical to have systems in place to find problems with coverage even after a claim has been rejected. Zee Medical Billing supports installing a coverage-detection safety net that can verify coverage post-denial. This proactive approach leads to an increase in overturned eligibility denials, a reduction in avoidable write-offs, and improved workflow efficiency.
Implement a Plan for Long-Term Improvement
At Zee Medical Billing, we understand that sustained success requires continuous improvement and evolution. To ensure ongoing success in denial prevention, we recommend implementing a comprehensive plan for long-term improvement.
Use Normalized Payer Data to Drive Workflow
Merely receiving responses from payers is not sufficient. Without normalization, staff members are forced to spend valuable time analyzing and interpreting each payer's unique remark codes. By driving workflows with normalized payer data, staff can work more efficiently and confidently, leading to improved outcomes and reduced denials.
Improve Processes Through Root Cause Analysis
To effectively address denials, it is essential to identify their root causes. Is the majority of denials coming from registration and eligibility issues? Missing data? Medical necessity requirements? Conducting root cause analysis enables organizations to pinpoint areas for improvement and implement targeted interventions, thereby maximizing denial prevention efforts.
Secure a Partner with Multi-Tiered Support
For healthcare companies, 73% of healthcare administrators agree that a lack of employees presents serious difficulties that lead to poor customer service and employee fatigue. Collaborating with suppliers that provide safe, multi-level support is essential to guaranteeing that employees can obtain resources and help in a timely manner when they encounter problems or difficulties. Empowering staff with the right tools and support can enhance productivity and decrease the impact of staffing shortages on denial prevention efforts.
Switch to a Single Platform
Fragmented healthcare payment systems can introduce friction and inefficiencies into denial prevention processes. Transitioning to a single, comprehensive platform streamlines workflows and removes barriers to success. While few revenue cycle solutions are truly complete, organizations can improve both staff and patient experiences by working with a vendor that provides a single platform and that can handle a variety of issues.





