The world is getting smaller and smaller as more people can communicate more easily and connect over networked computerized systems. Many gains are being made as various software and computer systems link up with one another for automated data sharing.
With so many complicated systems being networked together, problems of interoperability should be thought of by people working in all types of industries, with healthcare being no exemption.
What Is Interoperability?
Interoperability is the basic potential of computerized systems to connect and communicate with one another promptly, even if they were developed by extensively different manufacturers in different industries. The exchange of information between applications, databases, and other computer systems is essential for the modern economy.
According to the Healthcare Information and Management Systems Society, “Interoperability describes the extent to which systems and devices can exchange data, and interpret that shared data. For two systems to be interoperable, they must be able to exchange data and subsequently present that data such that it can be understood by a user.”
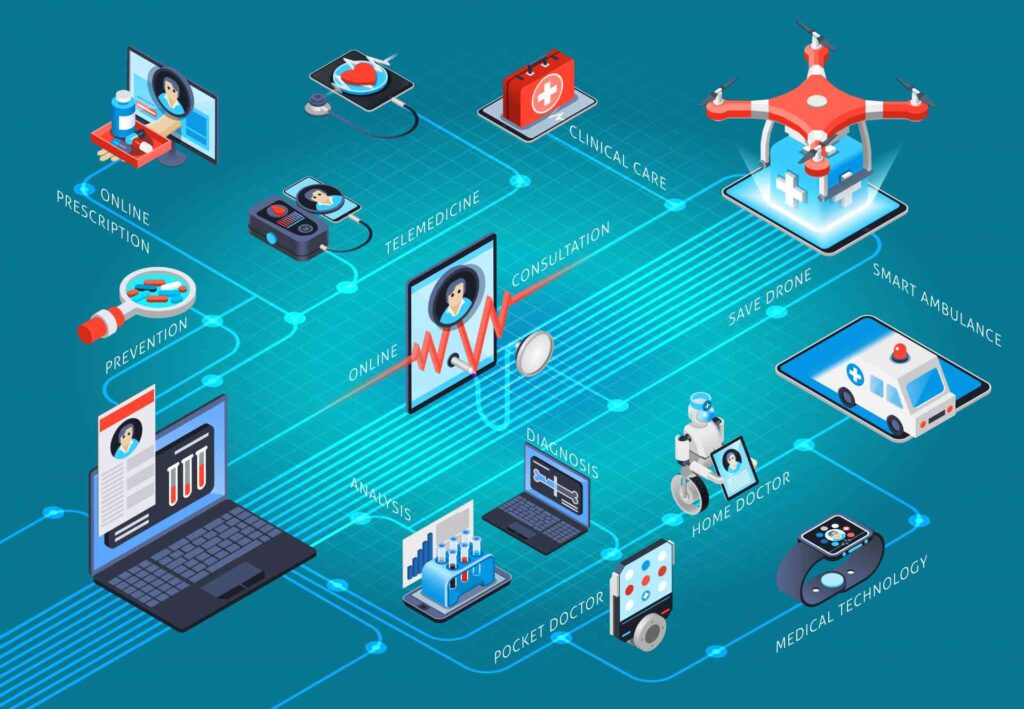
When we talk about the healthcare industry, interoperability has to do with the ability of different computer and software systems to exchange and share data from a range of alternative sources, including laboratories, clinics, pharmacies, hospitals, and medical practices.
The United States plays a role in interoperability in the healthcare industry by developing standards for how computer systems communicate and promoting particular standardized terms to define the systems and their connections. The government also establishes protocols for networking data, transmitting email, and improving other security and encryption schemes designed to safeguard confidential and sensitive patient information.
To further understand interoperability in healthcare let’s discuss three levels of health IT interoperability and learn more about the significance of this enhanced connectivity.
Three Levels of Healthcare Information Technology Interoperability
The HIMS board sets definitions for three levels of health information technology interoperability.
-
Foundational Interoperability
Foundational interoperability allows one information system to exchange data with another information system. The system receiving this information does not need to interpret the data and will be available for use instantly.
-
Structural Interoperability
Structural interoperability defines the format of the data exchange at an intermediate level. This has to do with standards that govern the format of messages being sent from one system to another. In such a way, the operational or clinical purpose of the information is evident and proceed through without alteration.
-
Semantic Interoperability
Semantic interoperability is the highest level of connection. Two or more different systems can exchange and use the information immediately. Here, the structure of the exchange of data and how the data itself is codified let medical providers share patient data even when using completely different EHR software solutions from different vendors.
It is significant not merely for cooperation amongst health care providers, but also for researchers and scientists who need large amounts of data to conduct studies on emerging diseases and other public health concerns.
Why Interoperability In Healthcare Is Important?
On the technical side of things, interoperability helps reduce the time it takes to have valuable conversations between providers as well as between doctors and their patients. This results in increased patient engagement and better outcomes as more time can be spent on the details of the illness or injury as the medical professionals come up with a treatment plan.
Interoperability in health care leads to access things easier like details in patients’ electronic health records, but it will only work to the extent that various medical software vendors will agree to share. What’s more, stakeholders in medical practices and other healthcare organizations must be willing to share patient details over networks for access by different databases.
Improved Efficiency
Interoperability in healthcare is designed to boost efficiency. When data is issued consistently no matter what the source, it’s easier for practitioners to quickly identify the matter and make treatment decisions.
Safer Transitions of Care
Interoperability enables safer transitions of care, which leads to better patient outcomes. For example, a patient who is on vacation and falls ill may not be able to provide all details of his medical history, which can make all the difference to the doctor charged with his care.
There was a highlight case where a heart patient from out of town was in the emergency room. He was only able to describe that he had undergone “some procedure”. The doctor would have been able to treat him faster if data from the patient’s electronic health record at his home state was accessible in another state.
Can Help Lower Costs
Interoperability is sharing of more helpful information promptly. Like, the patient’s blood test data of last week at his doctor’s office can be used today during a visit to an emergency room, saving them time and cost of doing more at the hospital. Improved performance through greater information sharing saves time and effort of staff, resulting in more cost savings.
It is important to recognize the importance of interoperability by professionals working in the healthcare industry. Many of our systems are connected over networks, we all need to stay on top of interoperability developments in government and industry.
For Queries about Interoperability in Healthcare __
Call @ +1 (224) 999-6997
Or
Get a free no-sting attached billing services quote from ZEE Medical Billing for your practice.