Medical credentialing is a market-driven process that seeks to keep standards of quality in the medical community for patient`s benefit. credentialing assures the patient that they are getting treated by a credible provider. It also helps physicians expand their business. Physicians/providers must credential themselves, i.e., enroll and attest with the payer’s network and get authorized to provide services to patients who are members of the payer’s plans.
So, if you want to free yourself from all the worries, piles of printed material, and perplexity with the insurance agencies. ZEE Medical Billing are credentialing specialists going above and beyond to explore the troublesome procedure of provider credentialing. ZEE Medical Billing gives providers credentialing administration at an unparalleled cost. Our service also incorporates a primary source check. We work on behalf of physicians and specialties at the same time.
Whether you want to get credentialed for insurance systems like Medicare, Medicaid, or commercial insurance payors, we can get you vetted as early as possible so that you start getting paid. Our arrangement fits any association paying little heed to their size or specialty. If you are an individual or a medical group, ZEE Medical Billing medical credentialing services would keep you updated efficiently.
What Is Medical Credentialing?
Credentialing is a term for a process that consists of two parts, credentialing and privileging. Credentialing is the verification of competency, as demonstrated by education, training, licensing and work experience. Privileging is the granting of approval for a healthcare provider to perform certain procedures based on the demonstration of competency.
The process involves direct contact with primary sources for the verification of a healthcare provider’s qualifications. The credentialing authority, called a Credentials Verification Organization or CVO, will contact the university where the provider received their degree in medicine, had their training, and did their residency, to confirm their credentials.
They will also contact certification boards and licensing agencies to verify licenses and specialty certificates. Hospitals and other employers can provide confirmation of work history. Credentialing is important for all new hires, but it is performed at regular intervals even after hiring to conform to the standards of regulatory and accrediting organizations, like The Joint Commission (TJC), The Centers for Medicare and Medicaid Services (CMS), and the National Committee for Quality Assurance (NCQA).
What Facilities Need Credentialing?
It is not only practitioners but facilities themselves that need to maintain standards of care and competence. The following kinds of facilities and services are obliged to acquire and maintain the proper credentials to act as healthcare providers include:
- Dialysis
- Ambulances
- Durable Medical Equipment
- Hospice Care
- Home Health Services
- In-Home Care Services
- Independent Diagnostic Testing
- IV Home Infusion Therapy
- Laboratories and Laboratory Collection Sites
- Prosthetics/Orthotics
- Radiology/Diagnostic Imaging
- Lithotripsy
Medical Credentialing Process
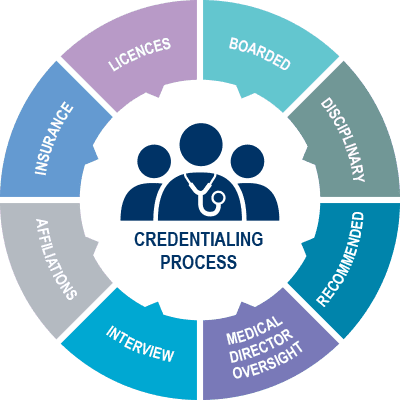
The credentialing process consists of verification and evaluation, followed by review and approval. A healthcare provider must wait until the credentialing process is complete and approved before they can begin to work. This assures that every patient, at all times, receives care from professionals who have the proper education, training, and experience to diagnose and treat their healthcare concerns. By allowing non-credentialed individuals to work, even if they are in the process of getting their credentials, a facility is putting itself at legal risk, as well as in jeopardy of losing its own credentials as an institution.
Credentialing is a primary process that verifies if the Provider satisfies the following criteria:
-
Has an unrestricted license
-
Any disciplinary actions or sanctions by insurers, hospitals, licensing boards, or professional organizations
-
Presence of any criminal history
-
Is the Provider certified by the medical board?
-
General health status
The credentialing process validates if a physician meets standards for delivering clinical care. It usually takes 60 – 120 days for a payer to get credentialed.
Medical Credentialing Checklist
The first step to success is good provider application in the credentialing process. A provider himself can fill this application, or he/she can outsource this process to an experienced Credentialing specialist. An accurate application will consist of all details, including:
-
Provider start date in practice
-
Copy of state license
-
Copy of DEA
-
Provider DOB and SSN
-
NPI #
-
Updated CV- work history
-
NPPES logons
-
CAQH logons
-
Malpractice incidence details
-
Copy of Degree/Diploma certificates
-
Copy of Driving License
-
Group Name
-
GNPI & Tax id
-
Practice and billing address along with Phone and Fax #
-
Signed W9
Medical Credentialing Costs
Medical credentialing costs vary from specialty to specialty, from facility to facility, and from CVO to CVO. Typically, an application fee of $200-$300 is not out of the ordinary. Often, facilities will offer reimbursements or partial reimbursements upon successful completion of credentialing.
If you are interested in using our credentialing services or want to find out more, contact us at (224) 999-6997.
OR
Get a free no-sting attached billing services quote from ZEE Medical Billing for your practice.