Table of Contents
ZEE Medical Billing's Strategy for Turning Challenges into Financial Success

Revenue cycle management is the most notable feature of healthcare companies. Healthcare providers face unique challenges at every point of the patient journey, from admission to post-care invoicing, which, if ignored, can result in significant revenue loss. As an experienced company from the last 2 decades, ZEE Medical Billing understands the significance of optimizing revenue cycles and turning lost revenue into gained revenue through strategic measures, analyzing trends, and taking preventative action, which will strengthen the revenue cycle and ensure the financial success of healthcare organizations. Let’s explore the four challenges that most organizations face in their Revenue cycle management process, raised by Zee Medical Billing in more detail, along with solutions.
Fulfilling Hospital Pricing Transparency Requirements
Enforcing compliance with expanded hospital price transparency requirements is one of the most significant challenges facing healthcare providers. As of 2021, legislative mandates dictate that hospitals must publicly disclose standardized charges, gross charges, and negotiated rates with payers in machine-readable formats. Hospitals must also provide cost prediction tools to patients for the top 300 shoppable services.
Leveraging Compliance for Financial Gain
At ZEE Medical Billing, we recognize that compliance with these regulations presents not only a challenge but also a significant opportunity for financial optimization. That’s why we offer a solution that requires healthcare organizations to prioritize compliance and use self-service estimating tools in order to efficiently meet these obligations and exploit them as avenues for revenue optimization.
Adherence to CMS updates, precise data reporting, open payment policies, and thorough payment estimates are all part of compliance. Adopting the most updated CMS templates is necessary to maintain compliance with changing regulatory standards and guarantee the correct posting of data components, payment methods, and anticipated payment amounts. Organizations need to make sure that patients are assured of their commitment to providing accurate and comprehensive information by adding an affirmation statement to this compliance endeavor. Transparency and trust among patients are enhanced when this information is easily available on the internet, complete with links to machine-readable text files.
Implementing Self-Service Estimation Tools
ZEE Medical billing places a high priority on accuracy since when your data is correct, your patients won’t experience any stress or uncertainty. For this reason, we suggest Healthcare providers implement user-friendly, market-tested self-service platforms that give precise estimates and real-time inquiry responses to provide patients with affordable tools. Given that approximately 65% of Americans worry about unforeseen bills, it’s critical to use a tool with automated features to help your patients feel more in control of their bills, improve their cash flows, and strengthen the relationship between patients and providers.
Enhance Protection: Three Pillars of Security Best Practices
Recognizing that businesses are frequently the target of security breaches caused by third-party vendors with excessive access rights, ZEE Medical Billing recommends that you push for an extensive yearly evaluation of vendor access. Due to their small size and possible lack of strong security measures, these businesses are more susceptible to cyberattacks.
Review of Vendor Access Every Year
Healthcare businesses can significantly lower the risk of data breaches by evaluating vendor access yearly, closely examining access levels, and ensuring that their security processes are in line with industry standards. Zee Medical Billing gives the following questions top priority as part of our thorough security evaluation.
- SOC 2 Compliance: Is the vendor certified to adhere to industry-standard security standards for protecting customer information, or does it lack this certification?
- Present Access Levels: Which suppliers presently have access to what parts of our network infrastructure?
- Access Optimization: Can suppliers carry out their tasks efficiently with fewer rights, reducing the possibility of security breaches?
Healthcare companies can enhance data protection and reduce the likelihood of external security risks by implementing strict security standards and proactively regulating vendor access.
Conducting a Cross-Functional Ransomware Tabletop Exercise
Traditional cybersecurity training methods frequently concentrate only on technical elements, ignoring the crucial part that cross-functional cooperation plays in making decisions quickly in emergency situations. ZEE Medical Billing proposes the use of a cross-functional ransomware tabletop exercise to close this gap.
This exercise simulates a real-life ransomware assault scenario, encouraging decision-makers from across departments to work together to address important problems and difficulties, as opposed to only evaluating technological capabilities. Here important areas of attention consist of:
- Making Crucial Decisions as an Executive: Executives are responsible for making crucial choices on things like whether to pay the ransom and how to handle data disclosure or deletion depending on response timings.
- Legal Review: Legal teams prepare communication strategies, evaluate liabilities, and examine the scope of compromise.
- Public Relations Strategy: PR departments create communication plans specifically for a range of stakeholders, including customers, suppliers, staff members, and members of the general public.
Through the proactive implementation of tabletop exercises, companies can identify any deficiencies in their decision-making procedures and enhance their reaction protocols, therefore efficiently reducing the impact of ransomware attacks.
Developing a Drawbridge Protocol to Facilitate B2B Exchanges
There are fundamental security issues associated with the widespread use of electronic connections with external parties in today’s linked digital world. For B2B connections, ZEE Medical Billing recommends implementing a drawbridge protocol in order to quickly respond to and reduce the risks resulting from breaches by third parties.
Some important factors to take into account when creating drawbridge procedures are:
- Procedure for Connection Removal: Creating a system to quickly terminate hacked connections when a third-party breach is discovered.
- Reinstatement Standards: establishing requirements for reconnections, such as confirming the nature of the infection and the length of the connection before the breach was discovered.
- Internal Breach Handling: Describes how to deal with internal breaches and isolate impacted systems quickly, especially in environments with many locations.
Prevent Denials: Four Key Junctures for Proactive Intervention
Research shows that over 60% of denials are caused by front-end problems, such as inaccurate modifiers, incomplete eligibility checks, and submission standards violations. In addition, differences related to permission account for over 40% of denials. Strong financial clearing systems that proactively handle front-end difficulties and reduce authorization-related risks are desperately needed, as these denial patterns highlight.
Top Causes for Claim Denials:
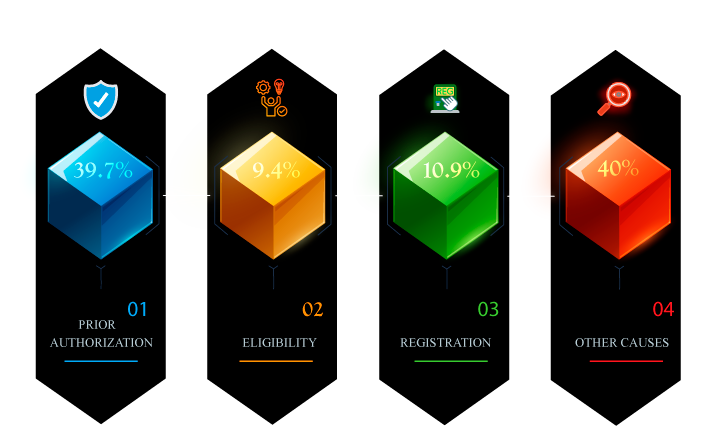
ZEE Medical Billing promotes proactive approaches that address fundamental causes of denials and streamline front-end operations to minimize denial risks and maximize revenue cycle performance. Healthcare companies can see denying difficulties as opportunities for progress by using the following strategies:
Locate Additional Active Insurance
Accurate and up-to-date insurance coverage data is critical, as registration and eligibility mistakes account for more than 20% of denials. The need for advanced software solutions is growing since traditional phishing techniques are no longer adequate to satisfy this need. These solutions provide:
- Autonomous Verification of Insurance Coverage: Software that automatically verifies active insurance coverage, irrespective of the patient’s point of entry.
- Enhanced Control: Systems that offer a high degree of control over patient coverage validation, guaranteeing precision and adherence.
- Customized Reporting: Systems that provide dashboards and reports that can be altered to improve insights and billing transparency.
Healthcare firms can enhance operational efficiency and drastically lower denial rates by automating coverage detection procedures.
Task by Exception
Taking a proactive approach to denial management is essential at a time when a large percentage of rejections remain unappealed. Companies should do these things:
- Leverage Robust Alerts: To rank claims with the highest likelihood of denial, employ exception-based workflows and robust alert systems.
- Employ Tools for Claim-Monitoring: Use claim monitoring tools to spot trends in each payer’s claim adjudications and expedite the appeals process.
- Harness Technology: To make well-informed decisions, examine past claim and remittance data using cutting-edge technology to determine projected cash value and overturn rates.
Healthcare businesses can improve revenue recovery and streamline rejection management procedures by utilizing software solutions to concentrate human efforts on claims that have the highest possibility of being paid.
Empower Managers with Insightful Data
Giving managers thorough data insights is crucial for gaining support for denial prevention initiatives from a variety of departments and clinical teams. ZEE Medical Billing advises building dashboards in real-time that enable managers to see account information, such as:
- Denial Rates: Monitor denial rates to spot patterns and areas that need work.
- Adjustment Codes: Examine adjustment codes to identify typical grounds for rejections.
- Write-offs: Evaluate write-offs to determine how much the company will lose financially from rejections.
Healthcare companies enable managers to determine the underlying reasons for denials and push for essential changes within their departments by providing them with access to comprehensive data. This evidence-based strategy speeds up the creation of action plans to address underlying problems and encourages a change toward proactive denial avoidance.
Make Payers accountable
ZEE Medical Billing stresses the significance of making payers accountable for their part in rejections and cash flow interruptions in addition to internal activities. It is recommended that healthcare organizations:
- Examine Contract Terms Frequently: Examine payer contracts on a regular basis to make sure they are in line with corporate goals and to find any differences that might affect revenue.
- Make Use of Payer Scorecards: Create payer scorecards to monitor performance indicators and identify potential problem areas throughout contract discussions.
- Report any irregularities. For a resolution, report any anomalies or unfair practices to the relevant advocacy groups or regulatory bodies.
- Strike Complex Deals: Make use of data insights to negotiate risk-based contracts that reduce payer-related risks and are in line with the organization’s financial objectives.
Healthcare companies can secure their bottom line and guarantee equitable payment for services provided by pushing for accountability and transparency in payer processes.
Ensuring Quality in Technology Implementation:
The potential for streamlining transactions from start to end and increasing operational effectiveness is enormous when artificial intelligence (AI) and machine learning (ML) are combined. However, careful planning, a strong technological foundation, and connection with corporate goals are essential for automation projects to succeed. At ZEE Medical Billing, we understand how critical it is to carry out exhaustive quality tests in order to guarantee the smooth implementation and efficacy of AI and ML solutions. When assessing the use of technology, keep the following four points in mind:
Scalability and Security of Technology
The democratization of access to AI and ML capabilities through technological breakthroughs makes it necessary to evaluate the security and scalability of implemented solutions. It is important for organizations to confirm that the technology they have selected can safely produce information and handle their data load. Important inquiries to make are as follows:
- Can Technology Be Scaled? Determine if the system can grow effectively to meet changing demands and manage the organization’s data load.
- What Safety Procedures Are Followed? Evaluate the strength of security measures to protect private patient information and guarantee adherence to legal requirements.
Scalability and security ensure that insights from AI and ML technologies are fully utilized, increasing their value to the organization.
Data Quantity and Quality
The quantity and quality of data sets used for training have a direct bearing on how well AI and ML models function. Leveraging large-scale data sets is essential for accurate insights and well-informed decision-making in healthcare revenue cycle management (RCM). Important things to think about are:
- Quantity of Available Data Sets: Examine the quantity and variety of the data sets that are accessible for ML and AI model training.
- Relevance and Data Coverage: Make sure the data sets are relevant to the particular goals of the firm and encompass a wide range of scenarios.
Organizations can improve the predictive power of AI and ML models and provide actionable insights to streamline revenue cycle operations by giving priority to both the quantity and quality of data.
Expertise and Use Case Identification
Successful implementation of AI and ML technologies requires deep subject matter expertise and a clear understanding of the intended use case. Organizations must identify key stakeholders and decision-makers who can provide domain-specific insights and guide the development and deployment of AI models. Key questions to consider include:
- Use Case Definition: Determine the specific use case for the AI model and identify the target users within the organization.
- Subject Matter Expertise: Assess the availability of subject matter experts who can provide insights into data interpretation and inform model development.
By engaging relevant stakeholders and subject matter experts from the outset, organizations can ensure that AI and ML initiatives are aligned with operational objectives and deliver actionable insights effectively.
Integration into Workflows and Execution
The real benefit of AI and ML technologies is how well they integrate into current operational procedures and workflows. To achieve significant results, organizations must create custom plans for integrating automation into operations. Key considerations include:
- Workflow Integration: determine how the automation of AI and ML will be integrated into the current procedures and workflows.
- Data-Driven Strategies: Find ways to use predictive insights to drive strategic decision-making and enhance results.
Through the prioritization of smooth execution and workflow integration, companies can fully leverage AI and ML technologies to improve patient outcomes and promote operational efficiency.





