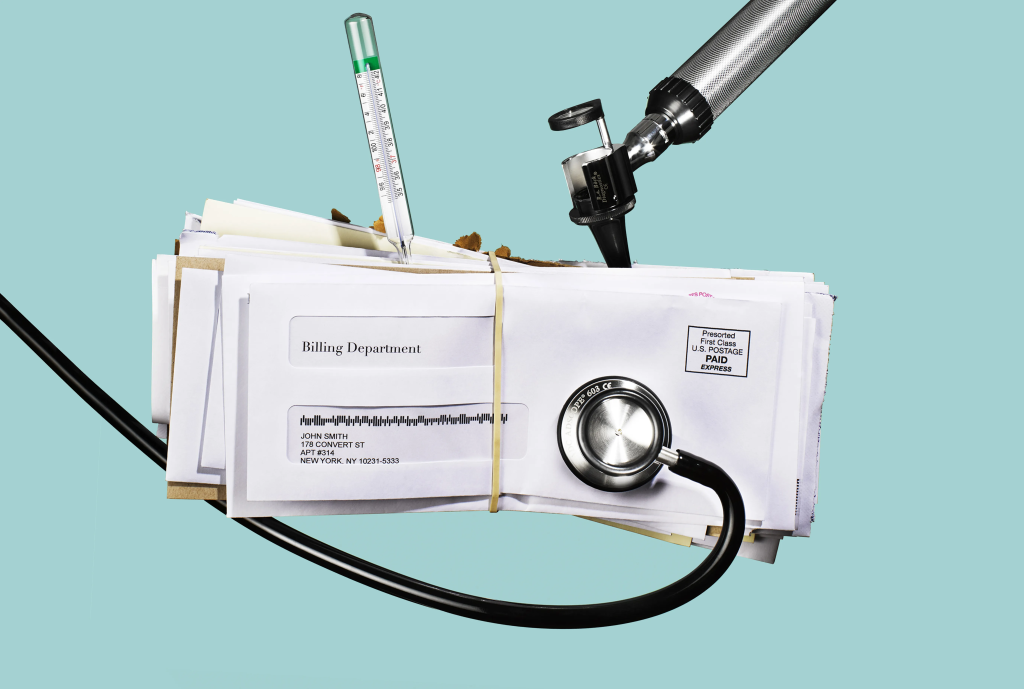
The Alarming Reality of Medical Billing Errors
Understanding the 80% Error Rate
The healthcare industry faces a staggering crisis: approximately 80% of medical bills contain errors. This alarming statistic represents billions of dollars in lost revenue and administrative burden for medical practices nationwide. At ZEE Medical Billing, we’ve analyzed thousands of claims and consistently found that most contain preventable mistakes ranging from simple data entry errors to complex coding inaccuracies.
These medical billing errors occur across all practice sizes and specialties. The errors span incorrect patient demographics, wrong insurance information, improper procedure codes, missing documentation, and compliance violations. Many practices remain unaware of their error rates until facing mounting denied claims and deteriorating cash flow.
The Financial Impact on Healthcare Practices
The financial consequences extend far beyond simple claim denials. Practices with high error rates typically experience claim denial rates between 15-20%, compared to best-in-class practices maintaining rates below 5%. Most practices forfeit between 7-11% of potential revenue due to billing mistakes alone.
Consider a practice generating $2 million annually: an 8% revenue loss equals $160,000 yearly. Beyond direct revenue loss, these errors create hidden costs. Staff spend countless hours correcting mistakes and resubmitting claims, diverting resources from patient care and practice growth.
Common Types of Medical Billing Errors
Medical Coding Accuracy Issues
Medical coding accuracy represents the most critical factor in clean claim submission. Common coding mistakes include using outdated codes, selecting non-specific codes when specific ones exist, failing to code to required specificity, incorrect diagnosis code sequencing, and missing secondary diagnoses. These errors result in claim denials, underpayments, and compliance violations. Our medical billing services prioritize accuracy through certified professional coders who maintain current credentials.
Patient Information Mistakes
Patient demographic errors account for significant preventable denials. These include misspelled names, incorrect birth dates, wrong insurance numbers, outdated coverage information, and inaccurate addresses. While seemingly trivial, these mistakes result in immediate rejections that delay payment. At ZEE Medical Billing, we implement robust verification processes that confirm accuracy before services are rendered.
Duplicate Billing and Unbundling Errors
Duplicate billing occurs when services are billed multiple times, often from inadequate charge capture systems. Payers view this with particular scrutiny as it can indicate fraudulent intent. Unbundling errors happen when procedures that should be billed together are instead billed separately, violating National Correct Coding Initiative rules. Proper revenue cycle management includes comprehensive checks identifying these issues before submission.
Healthcare Billing Compliance Violations
Healthcare billing compliance violations represent the most serious error category. Common issues include billing for medically unnecessary services, upcoding for higher reimbursement, billing for unrendered services, and failing to obtain required authorizations. These violations can result in refund demands, network exclusion, penalties, and prosecution. Our medical billing audit services examine compliance areas to identify potential violations before attracting regulatory attention.
Why Medical Billing Errors Happen So Frequently
Complex Coding Systems
Medical coding complexity has increased exponentially. The ICD-10 transition expanded codes from 13,000 to over 70,000 diagnosis codes. CPT codes receive annual updates with additions, revisions, and deletions. Each payer maintains unique requirements that vary from standard guidelines. This complexity creates an environment where even experienced coders struggle with accuracy. Practices maintaining high medical coding accuracy invest heavily in specialized expertise and ongoing education.
Staff Training Gaps
Many practices assign billing to staff lacking formal training. Common gaps include insufficient coding guideline understanding, unfamiliarity with payer requirements, inadequate compliance knowledge, and limited denial management experience. Staff turnover compounds this challenge, creating cycles of inconsistent quality that elevate error rates. Professional billing services eliminate this concern through stable, expert teams.
Outdated Revenue Cycle Management Systems
Legacy systems often lack modern error-prevention features including adequate claim scrubbing, real-time eligibility verification, comprehensive coding edits, and detailed analytics. Modern revenue cycle management requires sophisticated technology identifying errors before submission and providing insights for continuous improvement.
The Consequences of High Claim Denial Rates
Lost Revenue and Cash Flow Problems
High claim denial rates create immediate cash flow problems. When 15-20% of claims are initially denied, significant expected revenue fails to materialize. Studies show practices recover payment on only 60-70% of denied claims, meaning 30-40% result in permanent loss. For a practice submitting $200,000 monthly with a 15% denial rate and 35% permanent loss, this translates to over $125,000 in annual unrecoverable revenue.
Patient Satisfaction Decline
Medical billing errors directly impact satisfaction and reputation. Billing mistakes create confusion about patient responsibility, unexpected bills, and collection involvement. In today’s environment where satisfaction scores impact reimbursement and reviews influence growth, billing-related dissatisfaction creates consequences beyond individual errors. Practices with high error rates develop reputations deterring new patients.
Administrative Burden Increase
The administrative burden consumes productive staff time. Hours are spent weekly identifying denials, researching reasons, correcting errors, resubmitting claims, and managing patient questions. This creates a vicious cycle where consumed time prevents proactive error prevention, leading to more mistakes. Breaking this cycle requires systematic intervention to reduce billing mistakes.
How to Reduce Billing Mistakes in Your Practice
Invest in Regular Staff Training
Comprehensive training represents one of the most effective strategies to reduce billing mistakes. Training should address current coding guidelines, payer-specific requirements, documentation standards, compliance requirements, and denial management. We recommend monthly coding updates, quarterly comprehensive sessions, new staff orientation, immediate training on policy changes, and annual competency assessment.
Implement Advanced Billing Software
Modern software provides essential error-prevention tools including real-time eligibility verification, comprehensive claim scrubbing, automated coding suggestions, payer-specific edit checks, and denial tracking. When evaluating solutions, prioritize seamless EHR integration, robust reporting, regular updates, strong vendor support, and specialty-specific features.
Conduct Regular Medical Billing Audits
Regular medical billing audits provide visibility into accuracy and identify improvement opportunities. Audits should examine coding accuracy, documentation adequacy, charge capture completeness, denial patterns, and payer requirement compliance. We recommend comprehensive external audits annually with quarterly internal reviews.
The Role of Professional Medical Billing Services
Why Outsourcing Makes Sense
Professional medical billing services in USA offer compelling advantages including certified coding specialists, advanced technology without capital investment, denial management expertise, compliance monitoring, scalability without hiring challenges, and typically lower total cost. Practices that outsource typically experience claim denial rates dropping to 5% or below, decreased accounts receivable days, 15-30% collection increases, and staff redirection to patient-facing activities.
How ZEE Medical Billing Ensures Accuracy
At ZEE Medical Billing, we’ve developed comprehensive systems eliminating common medical billing errors. Our approach includes certified coders with current credentials, multi-level quality assurance with pre-submission review, real-time eligibility verification, comprehensive compliance monitoring, and sophisticated denial management. We specialize in revenue cycle management addressing every touchpoint from registration through payment posting.
Results speak for themselves: practices partnering with us experience dramatic improvements within 60-90 days. Our Get Your Free Billing Audit provides detailed current performance analysis and specific improvement recommendations.
Best Practices for Healthcare Billing Compliance
Maintaining healthcare billing compliance requires systematic approaches embedding compliance into daily operations. Best practices include establishing written policies, conducting regular training, implementing audit protocols, maintaining comprehensive documentation, designating a compliance officer, and creating a culture encouraging issue reporting.
Specific areas requiring attention include evaluation and management coding, modifier usage (especially modifier 25), medical necessity documentation, timely filing, coordination of benefits, and proper overpayment handling. Practices maintaining excellent compliance invest in education, implement strong controls, conduct regular audits, and address issues promptly.
Moving Your Practice into the 20%
Transitioning to the high-performing 20% requires commitment, investment, and systematic execution. The journey begins with honest assessment through comprehensive audit and analysis. Successful practices recognize billing accuracy as strategic priority, invest in expertise through staff development or professional services, implement preventive quality assurance, analyze performance regularly, and maintain continuous improvement.
Practices in the 20% category generate 15-30% more revenue from identical service volume, create better patient experiences, reduce administrative burden, and build professional reputations supporting growth.
Conclusion
The reality that 80% of medical bills contain errors represents both crisis and opportunity. While most practices struggle with high error rates draining revenue, the path to the elite 20% is clearly defined and achievable with proper commitment.
At ZEE Medical Billing, we’ve guided hundreds of practices through this transformation, delivering measurable results. The cost of inaction escalates as medical billing errors drain resources, reduce revenue, and create compliance risks. The tools and expertise exist to achieve consistently accurate billing maximizing revenue and ensuring compliance.
Contact ZEE Medical Billing today to Get Your Free Billing Audit and discover your path to billing excellence. Let us show you where errors cost revenue and how our medical billing services can transform your financial performance.
FAQs
1. What are the most common medical billing errors? Common medical billing errors include incorrect patient information, wrong insurance details, improper medical coding, missing modifiers, and lack of documentation.
2. How can I reduce my practice’s claim denial rate? Implement real-time eligibility verification, use certified coders, conduct pre-submission reviews, and analyze denial patterns. ZEE Medical Billing can reduce rates to 5% or below.
3. What is the average cost of billing errors? Practices lose 7-11% of potential revenue due to billing mistakes. For a $1 million practice, this means $70,000-$110,000 annually.
4. How often should my practice conduct billing audits? Conduct comprehensive medical billing audits annually with quarterly reviews of high-risk areas.
5. Should I outsource my medical billing? Outsourced services provide expert coders, advanced technology, and compliance monitoring, typically delivering 15-30% higher collections.
Follow Us
- Instagram: @zee_medical_billing
- Facebook: ZeeMedicalBilling
- YouTube: Zee Medical Billing Channel
- Twitter/X: @BillingZee
- LinkedIn: Zee Medical Billing Company