The landscape of behavioral health billing has evolved dramatically, presenting unique challenges that require specialized expertise. Unlike standard medical billing, behavioral health billing demand intricate knowledge of complex coding systems, varied treatment modalities, and ever-changing payer requirements that can significantly impact practice revenue.
Recent studies indicate that healthcare practices lose approximately $300 billion annually due to inefficient mental health billing processes. This staggering figure underscores the critical need for professional behavioral health billing that can navigate the complexities of this specialized field.
Key Challenges Facing Behavioral Health Billing Services

Complex Coding Systems in Behavioral Health Billing Services
Professional behavioral health billing must master specialized CPT codes that differ significantly from general medical procedures. The precision required is extraordinary – a simple time variation between 30-minute (CPT 90832) and 45-minute (CPT 90834) psychotherapy sessions can create substantial reimbursement differences over time.
Experienced behavioral health billing understand these nuances and implement systematic approaches to ensure accurate code selection, preventing costly reimbursement delays that can cripple practice cash flow.
Pre-Authorization Management Through Behavioral Health Billing Services
Securing pre-authorization remains one of the most time-intensive aspects of mental health practice management. Quality behavioral health billing streamline this process by maintaining detailed patient diagnosis records, comprehensive treatment plans, and all supporting documentation required by payers.
Professional services eliminate the administrative burden on healthcare providers, ensuring timely authorization approvals while maintaining compliance with payer-specific requirements.
Navigating Payer Regulations with Specialized Billing Services
Each insurance provider operates under distinct regulatory frameworks, creating a maze of requirements that practices must navigate. Expert behavioral health billing stay current with:
- Pre-authorization requirements across multiple payers
- State-specific coding standards and documentation needs
- Timely claim submission protocols
- Comprehensive denial management strategies
- Regulatory compliance updates and implementation
Managing Variable Treatment Plans
Mental health treatment inherently varies based on individual patient needs, making standardized billing approaches ineffective. Professional behavioral health billing develop flexible systems that accommodate diverse treatment scenarios while maintaining billing accuracy and compliance.
Essential Guidelines for Behavioral Health Billing Services
Universal Standards for All Behavioral Health Billing Services
Regardless of practice size or location, effective behavioral health billing must adhere to fundamental principles:
- Accurate CPT Code Implementation: Ensuring precise code selection for all services rendered
- Insurance Verification Protocols: Confirming coverage before treatment administration
- Pre-Authorization Management: Securing required approvals efficiently
- Comprehensive Documentation: Maintaining accurate, current, and complete records
- Timely Claim Submission: Meeting all payer deadlines consistently
- Regulatory Compliance: Staying current with federal and state requirement changes
CMS Compliance in Behavioral Health Billing Services
Centers for Medicare & Medicaid Services require behavioral health billing to demonstrate medical necessity for all covered treatments. Professional services ensure:
- Thorough documentation supporting medical necessity
- Proper provider credentialing for reimbursement eligibility
- Accurate coding and comprehensive documentation
- Full regulatory compliance across all claims
State-Specific Requirements for Behavioral Health Billing Services
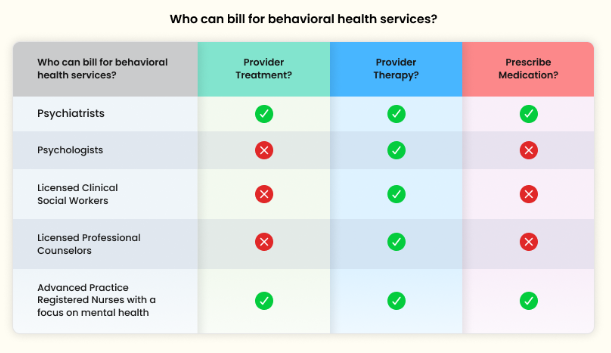
Medicaid coverage varies significantly between states, requiring specialized knowledge from behavioral health billing. For example:
- New York: Licensed social workers and mental health counselors qualify for Medicaid reimbursement
- Florida: Only licensed medical professionals like psychiatrists and psychologists are eligible
Professional behavioral health billing maintain current knowledge of state-specific regulations, telehealth requirements, licensing standards, and mental health parity laws.
Payer-Specific Guidelines in Behavioral Health Billing Services
Different payer types require distinct approaches:
- Medicare/Medicaid: Focus on medical necessity and state-specific requirements
- Private Insurance: Navigate plan-specific benefits and authorization processes
- Telehealth Services: Comply with evolving regulations and state-specific requirements
Most Utilized CPT Codes in Behavioral Health Billing Services
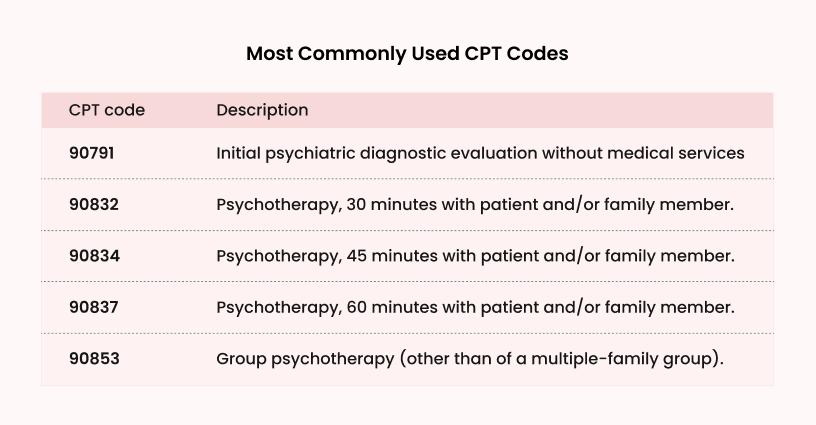
Professional behavioral health billing services frequently process these essential codes:
- Initial Psychiatric Diagnostic Evaluation
Used for the first meeting with a patient to assess their mental health, gather history, and create a treatment plan. No medical services (like prescribing medication) are included. - Psychotherapy
Covers a short therapy session (about half an hour) with the patient and/or their family member. Focuses on talking therapy and addressing specific issues. - Psychotherapy
A standard-length therapy session, most commonly billed. Allows deeper discussion of mental health concerns with the patient and/or family. - Psychotherapy
A longer therapy session, often for more complex cases or when extra time is needed to cover important topics in depth. - Group Psychotherapy
Used for sessions with multiple patients (not family-based), where participants work together under the therapist’s guidance to share experiences and support each other.
Best Practices for Behavioral Health Billing Services
Implementing Advanced EHR Systems
Modern behavioral health billing leverage sophisticated Electronic Health Record systems to minimize human error and streamline operations. These systems provide:
- Automated coding assistance and validation
- Real-time regulatory compliance checking
- Seamless data synchronization across platforms
- Enhanced inter-office coordination capabilities
- Comprehensive audit trails for compliance
Professional Behavioral Health Billing Services Advantages
Outsourcing to specialized behavioral health billing offers numerous benefits:
- Expertise and Compliance: Professional services maintain current knowledge of complex regulations and coding requirements
- Cost Efficiency: Reduces administrative overhead while improving claim approval rates
- Revenue Optimization: Faster reimbursements and reduced denial rates increase practice profitability
- Staff Relief: Eliminates administrative burnout, allowing staff to focus on patient care
- Technology Integration: Access to advanced billing software and AI-powered analytics
AI Integration in Behavioral Health Billing Services
Forward-thinking behavioral health billing utilize artificial intelligence for:
- Claims processing optimization and pattern analysis
- Denial reason identification and trending
- Reimbursement timeline analysis
- Process efficiency recommendations
- Predictive analytics for revenue cycle management
Effective Denial Management in Behavioral Health Billing Services
Common Denial Reasons
Professional behavioral health billing address frequent denial causes:
- Medical necessity documentation insufficient
- Incorrect or incomplete coding applications
- Missing pre-authorization requirements
- Inadequate supporting documentation
Proven Denial Prevention Strategies
Expert behavioral health billing services implement:
- Historical Analysis: Reviewing past denials to identify recurring patterns
- Staff Training: Continuous education on current regulations and best practices
- Verification Protocols: Confirming eligibility and authorization before treatment
- Documentation Standards: Maintaining detailed, accurate records for all services
Benefits of Professional Behavioral Health Billing Services
Improved Financial Outcomes
Specialized behavioral health billing deliver:
- Reduced Coding Errors: Professional expertise minimizes claim rejections
- Streamlined Authorization: Efficient pre-authorization processes reduce delays
- Centralized Management: Multi-location practices benefit from unified billing systems
- Automated Processes: Reduced human error through technology integration
- Enhanced Cash Flow: Faster reimbursements improve practice financial stability
Operational Efficiency
Professional services provide:
- Administrative Relief: Staff can focus on patient care rather than billing complexities
- Scalability: Services adapt to practice growth and changing needs
- Compliance Assurance: Expert knowledge ensures regulatory adherence
- Technology Access: Advanced tools and software without capital investment
Choosing the Right Behavioral Health Billing Services Partner
When selecting Mental health billing services, consider providers that offer:
Comprehensive Service Portfolios
- Complete revenue cycle management
- Insurance verification and authorization
- Claims processing and submission
- Denial management and appeals
- Compliance monitoring and reporting
Technology Integration
- Advanced EHR system compatibility
- Real-time reporting and analytics
- Automated workflow management
- AI-powered optimization tools
Industry Expertise
- Specialized behavioral health knowledge
- Current regulatory compliance understanding
- Multi-payer experience and relationships
- Proven track record with similar practices
Ready to Transform Your Behavioral Health Practice Revenue?
Don’t let complex billing challenges limit your ability to serve patients. Zee Medical Billing specializes in behavioral health billing with proven expertise in mental health, psychiatry, psychology, and counseling practices.
✅ 99% Clean Submission Rate – Industry-leading accuracy
✅ 30% Average Revenue Increase – Proven results
✅ Rates as Low as 2.49% – Competitive pricing
✅ Zero Upfront Costs – No financial risk
✅ 7+ Years Mental Health Experience – Specialized expertise
Get Your Free Behavioral Health Billing Assessment →
Join 1000+ behavioral health providers who trust Zee Medical Billing
The Future of Behavioral Health Billing Services
As mental health awareness continues growing, the demand for efficient behavioral health billing will expand. Practices that partner with professional services position themselves for:
- Improved Patient Access: Streamlined billing reduces barriers to care
- Financial Stability: Optimized revenue cycles support practice growth
- Operational Efficiency: Advanced systems free resources for patient care
- Regulatory Compliance: Expert knowledge ensures adherence to evolving requirements
Conclusion
Navigating the complex world of behavioral health billing services doesn’t have to be overwhelming. The key is understanding that mental health billing requires specialized expertise, advanced technology, and dedicated focus that most practices can’t maintain internally while still providing excellent patient care.
Professional behavioral health billing services offer the knowledge, tools, and efficiency needed to optimize your revenue cycle while ensuring compliance with ever-changing regulations. As the mental health field continues to evolve, partnering with specialists like Zee Medical Billing becomes increasingly essential for practice success and sustainability.
Remember, investing in quality behavioral health billing services isn’t just a financial decision – it’s a commitment to your practice’s future and your ability to serve patients effectively for years to come.
Frequently Asked Questions About Behavioral Health Billing Services
1. What are behavioral health billing?
Behavioral health billing are specialized medical billing solutions for mental health providers. They handle complex coding, insurance verification, claims processing, and revenue cycle management specific to behavioral healthcare practices.
2. How much do behavioral health billing services cost?
Most mental health billing services charge 4-8% of collected revenue. Despite this cost, practices typically see 15-30% revenue increases through improved claim acceptance rates and faster reimbursements.
3. What CPT codes do behavioral health billing handle?
Professional services commonly process codes like 90791 (psychiatric evaluation), 90834 (45-minute therapy), 90837 (60-minute therapy), 90847 (family therapy), and 90853 (group therapy), along with various mental health diagnostic codes.
4. How long does it take to see results from outsourced billing services?
Most practices see improvements within 30-60 days, including faster claim processing. Long-term benefits like improved denial rates and optimized revenue cycles typically develop over 3-6 months.
5. Can behavioral health billing services help reduce claim denials?
Yes, professional services include comprehensive denial management and appeals processes. They typically achieve 85-95% first-pass claim approval rates compared to 65-75% for in-house billing operations.
Follow Us
Stay updated with the latest behavioral health billing insights, industry trends, and regulatory changes by following Zee Medical Billing on our social media channels:
- Instagram: @zee_medical_billing
- Facebook: ZeeMedicalBilling
- YouTube: Zee Medical Billing Channel
- Twitter/X: @BillingZee
- LinkedIn: Zee Medical Billing Company