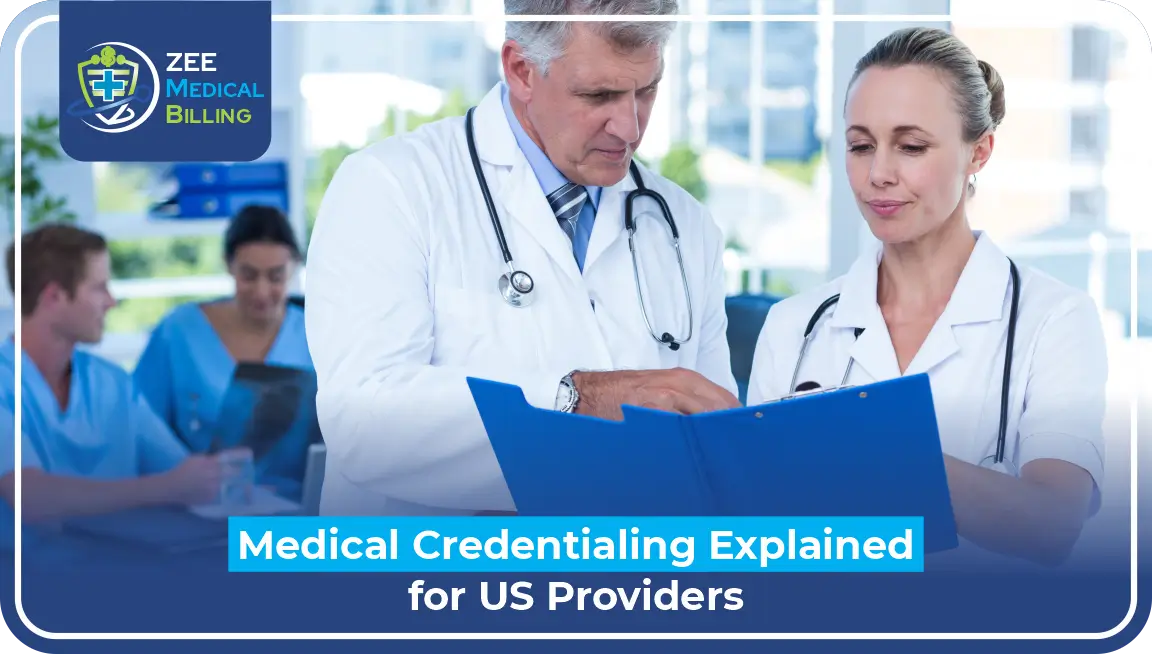
Credentialing is the method involved with joining an insurance plan’s organization so you can serve clients covered by their health plans.
Additionally called “paneling” or becoming “in-network,” credentialing can open your administrations to additional clients and assist you with finishing up your caseload.
Here are the means you want to take to get your confidential practice credentialed, from picking insurance plans to understanding timelines.
Why is Credentialing Important?
Before an insurer can get your organization and send its individuals to your training — it needs to affirm you’re authorized and trained to give care.
However, it’s a two-way road. During the cycle, you can survey how the insurance plan carries on with work, including their fee schedule.
The timetable lets you know the amount you’ll be repaid by the insurer for the administrations you give insured clients.
So, getting credentialed is an opportunity for both you and the guarantor to find out about each other, and conclude whether an expert relationship would be valuable together.
The importance of medical billing credentialing in healthcare
Medical Billing credentialing is an important cycle that guarantees medical care suppliers satisfy industry guidelines and administrative necessities. By checking capabilities and accreditations, this interaction limits billing errors upgrades consistency, and encourages trust among suppliers and payers. Focusing on credentialing not only protects income but also supports great patient care. Invest in credentialing to reinforce your practice’s foundation!
At Zee Medical Billing, we deal with each step with accuracy to guarantee precision and quicker repayments and credentialing.
Advantages of Proper Credentialing
Being credentialed isn’t equivalent to being authorized. In the US, a medical license shows that you have:
- Passed your state’s medical boards
- The suitable information and instruction to practice medicine
- The option to be known as a physician
Some insurance companies, including Medicare, require extra, checked data, including data about malpractice claims, to consider you a protected and trusted medical care supplier for their individuals formally.
By getting a certificate from numerous medical coverage organizations, you gain the ability to submit claims for a different cluster of therapies and quickly get repayment.
Credentialed suppliers can grow their patient base by tolerating an assortment of protection plans, in this way expanding practice income. Being recorded on protection sites as an in-network supplier further develops visibility and credibility, drawing in additional patients. Insurance credentialing also assists suppliers with getting a more extensive number of protection benefits for their patients, upgrading the affordability and accessibility of medical care administrations.
In addition, credentialing smoothed out regulatory assignments, diminishing the above costs related to billing and guarantee handling. Being credentialed with protection plans can in a roundabout way influence patients’ protection deductible costs by giving them admittance to cheaper medical care administrations inside their protection organization. Eventually, it works with better understanding consideration by guaranteeing consistent coordination with protection transporters.
Process For Insurance Credentialing
Here is an overview of the process:
1. Research and Preparation
Understand Requirements: Different protection boards (e.g., Aetna, Blue Cross Blue Shield, Cigna) may have various necessities, so exploring everyone’s criteria is important.
Gather Essential Documentation: Typical documentation incorporates:
- A present status license (psychologist, therapist, clinical social worker, and so forth.)
- Professional liability insurance
- National Supplier Identifier (NPI)
- CAQH (Council for Reasonable Quality Healthcare) ID — most insurance agencies require this
- Proof of education and training (e.g., confirmations, certificates of completion, records)
- Work history and references.
2. Complete a CAQH Application
- CAQH fills in as a centralized data set where you enter your professional and practice data, which numerous insurance agencies access during the credentialing system.
- Make a CAQH ProView account and enter subtleties like your schooling, training, work history, malpractice history, and license.
- Update the CAQH profile routinely and guarantee that it is exact and finished. Insurance agencies will require your profile to be dynamic and updated to handle your application.
3. Submit Applications to Insurance Companies
- Direct Application: Apply straightforwardly to the protection boards you wish to join, typically through their supplier gateway or a particular contact email.
- Every insurance agency has its application interaction. Some might have structures that should be filled up and emailed back, while others have online applications.
- Incorporate CAQH Number: While applying to insurance companies, incorporate your CAQH ID to smooth out the cycle.
4. Background Check and Confirmation
- Essential Source Verification: Insurance companies will check your credentials, including your state license, training, work history, and any disciplinary activities.
- They may also survey your malpractice history and request references from colleagues.
- This verification cycle can require a little while or months, depending on the insurance company’s methodology.
5. Contract Review and Negotiation
- When the insurance company finishes the confirmation, you’ll get a supplier understanding or contract.
- Review the agreement completely for details concerning reimbursement rates, covered administrations, billing methodology, and dispute resolution.
- If you have concerns or wish to arrange reimbursement rates, you can endeavor to negotiate, but the progress of negotiations can change given the insurer’s policies.
6. Get In-Network Status
- After signing the contract, the insurance company will deal with the understanding, and you will be viewed as an in-network supplier.
- You will get a provider number and guidelines on the most proficient method to submit claims to the insurance company.
- Once credentialed, you can begin accepting patients with that protection and billing the insurance company straightforwardly.
7. Recredentialing
- Insurance companies commonly expect suppliers to go through a credentialing interaction every few years.
- This cycle includes refreshing any progressions in your training, education, or different certifications and guaranteeing that you stay on favorable terms with your licensing board.
- Keeping your CAQH profile updated will work with a smoother credentialing process.
Timeline of the Process
The whole credentialing cycle can take somewhere in the range of 60 to 180 days. Delays are normal if there are missing documents or mistakes in the application. Being exhaustive and responsive to any solicitations for extra data can assist with accelerating the interaction.
Bottom Line
Insurance credentialing is important for advisors keen on working with insurance companies. It gives prospects, for example, an extended client base, greater reliability, and financial stability. Signing up for protection boards is a difficult process. However, the rewards might offset the initial efforts. Therapists can set up a good foundation for themselves as reputable providers in the health industry by taking suitable techniques.