.Medicare has certain rules and regulations in place to prevent fraud, waste, and abuse. Here’s one you may have heard of – the 8-minute rule. As a Medicare beneficiary, it’s helpful to be acquainted with terms such as Medicare’s “8-minute rule” to understand how Medicare gets charged for the services. Due to the limited understanding regarding this rule, errors occasionally happen which results in delayed reimbursement or underbilling.
Let’s understand the Medicare 8-Minute Rule for Physical Therapy Billing with Zee Medical Billing. In this providers must treat patients for at least eight minutes to receive Medicare reimbursement.
What Is Medicare’s 8-Minute Rule?
Physical therapy billing guidelines for Medicare and Medicaid services include a section about how much time you must spend with a patient for it to be “bill-worthy.” Medicare physical therapy billing works in increments of 15. So what are you supposed to do when your treatment only takes 13 minutes to complete?
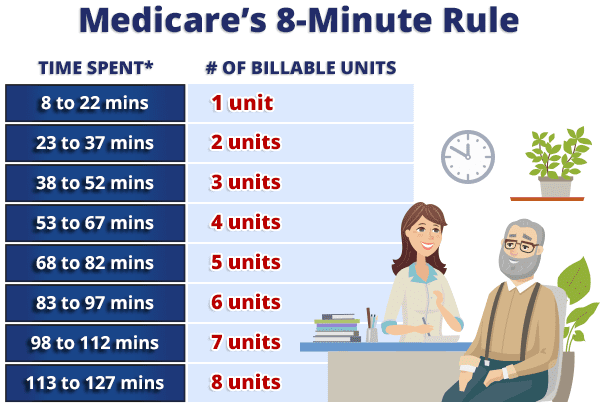
That’s where the eight-minute rule comes in. You only have to spend eight minutes with a patient to be able to bill for one “15-minute” unit. However, if you spend 16 minutes with a patient, you’ll still only be able to bill for one unit. You’d have to spend 23 minutes with a patient to be able to fall into the two-unit bracket.
How Does Medicare 8 Minute Rule for Physical Therapy Work?
The 8-minute rule states that you must provide treatment for at least eight minutes to receive Medicare reimbursement. Using the “rule of eights,” billing units that are normally based on 15-minute increments spent with a patient can be regulated. One must complete at least eight minutes of treatment be paid for one 15-minutes increment.
For example, after completing 17 minutes of treatment, Medicare would be billed for 15 minutes or one unit. However, if you completed 23 minutes of treatment, Medicare would be billed for two units of treatment. Even if you spent 23 or 30 minutes with the patient the bill would still be for two units.
Guidelines for when Medicare 8-minute Rule for Physical Therapy Applies
Medicare’s 8-minute rule is a condition that applies to time-based CPT codes for outpatient services. The rule allows practitioners to bill Medicare for one unit of service if its length is at least eight but less than 22 minutes. A billable “unit” of service refers to the time interval for the service provided. Under the 8-minute rule, each unit of service consists of 15 minutes.
Billable units for the eight-minute rule would look something like this:
If you perform physical therapy with a patient for only five minutes, the timer resets before you begin the next activity. You cannot bill Medicare until you have worked with a patient on one activity for at least eight minutes.
Current Procedural Terminology (CPT) Codes
CPT codes describe the procedures and services you are performing to billing agencies and insurance companies. They were created by the American Medical Association in 1966 to simplify and standardize reporting of procedures.
There are three code categories and each code consists of five characters:
- Category 1 → services and procedures
- Category 2 → performance management
- Category 3 → emerging and experimental services and procedures
Each category can be divided into sections.
Category one contains:
- Anesthesia (numbers 01000-01999)
- Surgery (numbers 10021-69990)
- Radiology (numbers 70010-79999)
- Pathology and labs (numbers 80047-89298)
- Medical services/procedures (numbers 90281-99607)
- Evaluation and management services (numbers 99201 through 99499)
Category two contains:
- Composite measures (numbers 0001F-0015F)
- Patient management (numbers 0500F-0584F)
- Patient history (numbers 1000F-1505F)
- Physical exams (numbers 2000F-2060F)
- Diagnostics/screenings (numbers 3006F-3776F)
- Therapy/Preventive/Other interventions (numbers 4000F-4563F)
- Patient safety (numbers 6005F-6150F)
- Structural measures (numbers 7010F-7025F)
- Nonmeasure code listing (numbers 9001F-9007F)
Category three codes:
Category three codes are temporary and contain four numbers, followed by the letter “T.”
Physical therapy codes can be divided into service-based and time-based codes.
What are Service-Based CPT Codes?
Service-based CPT codes are:
Hot/cold packs → 97010
Physical Therapy Evaluations → 97161, 97162, 97163
Unattended Electrical Stimulation → 97014
What Are Time-Based CPT Codes?
Time-based CPT codes are as follows:
Ultrasound → 97035
Manual Therapy → 97140
Therapeutic Exercise → 97110
Therapeutic Activities → 97530
Neuromuscular Re-education → 97112
Gait Training → 97116
Iontophoresis → 97033
Manual Electrical Stimulation → 97032
Time-Based vs. Service-Based CPT Codes
CPT time-based coding is different from CPT Service-based billing guidelines. Let us make clear how the eight-minute rule works for minimal services, like applying cold compresses or completing a brief examination. These services are not time-based means you can only bill one unit regardless of whether it takes you 15 or 23 minutes to complete all of those minor components.
Billing gets tricky where you’ll need to use time-based units only for one-on-one, “constant attendance procedures.” Like when you spend 25 minutes on a patient’s initial exam. During this time, you and your staff are asking questions, physically examining the affected area, etc. After that, you spend 20 minutes one-on-one with the patient performing a physical therapy exercise. Technically, you’ve spent 45 minutes with the patient, which would equate to three billing units. But, those first 25 minutes only counted for one unit because you were not in the room for the whole time, and you were not performing one undivided task. Hence, you can only bill for two units.
Does The 8-minute Rule Apply to All Insurances?
By definition, the 8-minute rule applies to Medicare, Medicaid, TRICARE, and CHAMPUS. Private insurance carriers may choose to operate the same way, but by rule are not required to. Medicare beneficiaries who enroll in private Medicare plans (Medicare Advantage) may also have different billing standards depending on the plan.
AMA 8-Minute Rule & The Rule of Eights
AMA 8-Minute Rule is found within the CPT code manual. This CPT rule is somewhat different from the CMS rule for Medicare and Medicaid.
The overall concept is the same – billing occurs in 15-minute increments, with over eight minutes of service counting for one 15-minute increment. However, time is not combined. There are no mixed remainders. Each 15-minute increment of service is treated as if it is billed separately.
This AMA timed code means that if you perform one physical therapy service for 16 minutes, and another for 22, you’d only bill for two units, instead of combining the extra one minute from the 16-minute service and the extra seven minutes from the 22-minute service to create a third unit.
How to Avoid Mistakes of 8-Minute Rule for Physical Therapy with ZMB?
Considering that it took us over 1,000 words to explain this one billing process, it can be pretty easy to perform incorrectly. We recommend NOT trying to do the math yourself for every patient. We at Zee Medical Billing will do all this for you. We can help you with all your billing tasks and whatever your practice needs so you can’t mess up the eight-minute rule.
For Queries__
Call @ +1 (224) 999-6997
Or
Get a free no-sting attached billing services quote from ZEE Medical Billing for your practice.